Is Coffee Low FODMAP? Your Complete Guide to Safe Sips

Quick Answer
Yes, black coffee is low FODMAP according to Monash University research. Pure coffee contains no FODMAP carbohydrates, making it suitable for the low FODMAP diet when consumed in moderate portions (small espresso or small brewed coffee serving). For a deeper dive into what you can drink on a low FODMAP diet, see this authoritative guide.
Key Takeaways
- Black coffee is low FODMAP according to Monash University research.
- Pure coffee contains no FODMAP carbohydrates.
- Black coffee is suitable for the low FODMAP diet when consumed in moderate portions.
- Recommended serving sizes include a small espresso or a small brewed coffee.
Coffee and the Low FODMAP Diet: The Basics
If you're navigating IBS symptoms or digestive sensitivities, you've probably wondered whether your morning coffee ritual needs to change. The good news? Black coffee is considered low FODMAP, which means you don't have to give up your favorite brew entirely. But there's more to the story than just the coffee itself.
Understanding how coffee fits into a gut-friendly lifestyle requires looking at both the FODMAP content and other factors that might trigger digestive discomfort. Let's break down everything you need to know about coffee and FODMAPs. For more on how coffee interacts with IBS, check out this in-depth discussion.
What is the FODMAP Diet?
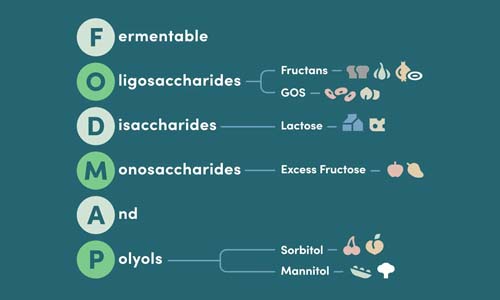
The low FODMAP diet targets specific fermentable carbohydrates that can trigger IBS symptoms in sensitive individuals. FODMAP stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols—a group of short-chain carbohydrates that are poorly absorbed in the small intestine.
Key Fact: Two-thirds of Americans experience digestive issues, and nearly 1 billion people worldwide live with IBS, making the low FODMAP approach increasingly relevant for digestive comfort.
The diet works in two phases:
- Elimination Phase: Remove high FODMAP foods for 2-6 weeks to calm symptoms
- Reintroduction Phase: Gradually test individual FODMAP groups to identify personal triggers and tolerance levels
This systematic approach helps you create a personalized eating plan that maximizes both digestive comfort and food variety.
Is Coffee Low FODMAP?
Black coffee is considered low FODMAP by both Monash University (the leading FODMAP research authority) and current scientific consensus. Pure coffee contains no FODMAP carbohydrates, making it suitable for the elimination phase of the diet.
Here's what makes coffee low FODMAP:
- Pure coffee beans contain no fermentable carbohydrates
- The brewing process doesn't add FODMAP compounds
- Black coffee, espresso, and instant coffee (100% coffee bean) are all low FODMAP options
Important Distinction: Being low FODMAP doesn't mean coffee won't trigger IBS symptoms. Coffee can still cause digestive discomfort due to caffeine and other compounds—this is separate from FODMAP content.
The confusion often arises because people experience digestive symptoms after drinking coffee and assume it's high FODMAP. In reality, coffee's stimulant properties and acidity can trigger symptoms through different mechanisms than FODMAPs.
How Much Coffee is Low FODMAP?
While coffee itself is low FODMAP, portion size still matters. Research indicates that a small espresso or small brewed coffee serving maintains low FODMAP status. Here's what you need to know about serving sizes:
- Small Espresso (30ml/1 oz)
- Considered low FODMAP and the safest starting point
- Small Brewed Coffee (250ml/1 cup)
- Generally low FODMAP, but individual tolerance varies
- Large Servings
- May increase FODMAP content and are more likely to trigger symptoms
The key principle: start small and monitor your body's response. Even low FODMAP foods can cause issues when consumed in large quantities, and coffee's stimulant effects become more pronounced with larger servings. For a comprehensive look at coffee drinks and FODMAPs, see this detailed resource.
Coffee, IBS, and Gut Sensitivity
Understanding coffee's relationship with IBS goes beyond FODMAP content. Even though coffee is low FODMAP, it can still trigger digestive symptoms through other mechanisms. This is crucial information for anyone managing IBS or gut sensitivities.
The Role of Caffeine in IBS
Caffeine acts as a potential IBS symptom trigger independent of FODMAP content. Here's how caffeine affects your digestive system:
Caffeine's Gut Effects
- Increased gastric motility: Speeds up digestion and bowel movements
- Stimulates gastric acid production: Can worsen acid reflux and stomach irritation
- Triggers gastrocolic reflex: The urge to have a bowel movement after eating/drinking
- Affects nervous system: Can increase anxiety, which worsens IBS symptoms
The impact varies significantly based on your IBS type:
- IBS-D (Diarrhea-predominant)
- Coffee may worsen symptoms by increasing bowel movement frequency and urgency
- IBS-C (Constipation-predominant)
- Some people find coffee helpful for stimulating bowel movements, though this varies individually
- IBS-M (Mixed)
- Effects can be unpredictable and may vary day to day
"In our experience helping customers navigate gut sensitivities, we've found that coffee tolerance is highly individual. Some people with IBS enjoy coffee without issues, while others find even small amounts triggering—regardless of FODMAP content."
Other Gut Effects: Heartburn, Reflux, and Indigestion
Coffee's effects on digestion extend beyond IBS symptoms. The beverage can increase stomach acid production and aggravate gastroesophageal reflux disease (GERD) or general heartburn.
Research suggests multiple compounds in coffee contribute to these effects:
- Caffeine: Stimulates acid production and can relax the lower esophageal sphincter
- Chlorogenic acids: Bitter compounds that may increase gastric acid secretion
- N-alkanoyl-5-hydroxytryptamides: Compounds that stimulate stomach acid production
Interestingly, decaffeinated coffee can still trigger acid reflux in some people, suggesting that caffeine isn't the only culprit. The roasting process and other naturally occurring compounds play a role too.
Sensitivity is Personal
One of the most important things to understand about coffee and IBS is that individual tolerance varies dramatically. Some people with diagnosed IBS enjoy multiple cups daily without issues, while others experience symptoms from even small amounts.
Factors that influence coffee tolerance include:
- Genetics: Caffeine metabolism varies based on genetic factors
- Stress levels: High stress can amplify coffee's gut-stimulating effects
- Timing: Coffee on an empty stomach often causes more issues
- Overall diet: Other trigger foods can compound coffee's effects
- Sleep quality: Poor sleep can increase sensitivity to caffeine
Professional Guidance: If you're unsure about your coffee tolerance, consider working with a FODMAP-trained dietitian. They can help you systematically test coffee while monitoring symptoms through a detailed food and symptom diary.
The best approach is to start with small amounts and track your body's response. Keep a symptom diary noting the type of coffee, amount consumed, timing, and any digestive symptoms that follow. This data helps you identify your personal tolerance level and optimal consumption patterns.
How Coffee Becomes High FODMAP
 fodmap coffee creamers">
fodmap coffee creamers">
While pure coffee is low FODMAP, many coffee drinks become problematic when you add certain ingredients. Understanding which additives raise FODMAP content helps you make informed choices about your daily brew.
The transformation from low FODMAP to high FODMAP happens with what you add to your coffee, not the coffee itself. Most coffee-related digestive issues stem from dairy milk, sweeteners, and flavored syrups.
Additives That Raise FODMAP Content
Several common coffee additions can quickly turn your low FODMAP beverage into a trigger for digestive discomfort:
- Regular Dairy Milk
- Contains lactose, a high FODMAP disaccharide that many people struggle to digest properly
- Soy Milk (whole soybean-based)
- Traditional soy milk made from whole soybeans contains oligosaccharides, though soy protein-based alternatives are low FODMAP
- Flavored Syrups
- Often contain high fructose corn syrup, honey, or other high FODMAP sweeteners
- Artificial Creamers
- May contain lactose, inulin, or other high FODMAP fibers used as thickeners
High FODMAP Coffee Additions to Avoid
- Regular cow's milk (lactose)
- Whole soybean-based soy milk
- Honey and agave nectar
- High fructose corn syrup
- Inulin-containing creamers
- Coconut milk in large quantities
Low FODMAP Ways to Enjoy Coffee
The good news is that plenty of delicious options keep your coffee both flavorful and gut-friendly. Here are the best low FODMAP alternatives:
Safe Milk Alternatives: Lactose-free milk, almond milk, macadamia milk, and soy protein-based milk are all excellent low FODMAP options that add creaminess without digestive discomfort.
| Ingredient | FODMAP Status | Serving Size | Notes |
|---|---|---|---|
| Lactose-free milk | Low FODMAP | 1 cup (250ml) | Tastes most like regular milk |
| Almond milk | Low FODMAP | 1 cup (250ml) | Light, nutty flavor |
| Macadamia milk | Low FODMAP | 1 cup (250ml) | Creamy, rich texture |
| Regular sugar | Low FODMAP | 2 tablespoons | Simple and reliable |
| Maple syrup | Low FODMAP | 2 tablespoons | Natural sweetness |
For sweetening, regular sugar remains your safest bet. It's low FODMAP and doesn't add any digestive complications. Avoid honey, agave nectar, and artificial sweeteners containing sorbitol, mannitol, or inulin.
Decaf Option: Decaffeinated coffee is also low FODMAP and may be a better choice if you're sensitive to caffeine's gut-stimulating effects while still wanting to enjoy coffee's flavor.
Coffee Preparation Methods and Tolerance
Different brewing methods can affect how well you tolerate coffee, even though they're all low FODMAP when prepared with safe ingredients:
- Black coffee: Lowest risk option, no additives to worry about
- Espresso: Concentrated but small serving size, often well-tolerated
- Cold brew: Lower acidity may be gentler on sensitive stomachs
- Instant coffee: Choose 100% coffee bean varieties, avoid blends with chicory
The brewing method itself doesn't change FODMAP content, but it can affect acidity levels and caffeine concentration, which may influence your individual tolerance.
Practical Tips for Coffee Lovers on a Low FODMAP Diet

Navigating coffee choices while following a low FODMAP diet doesn't have to be complicated. With the right strategies, you can continue enjoying your favorite beverage both at home and when you're out and about.
At Home
Creating the perfect low FODMAP coffee routine at home gives you complete control over ingredients and preparation methods:
"We recommend starting with high-quality, 100% pure coffee beans and building your perfect cup from there. This approach ensures you're getting the cleanest flavor without any hidden additives that might trigger symptoms."
- Choose pure coffee: Select 100% coffee beans or ground coffee without additives
- Monitor portion sizes: Start with small servings and adjust based on tolerance
- Stock low FODMAP milk alternatives: Keep lactose-free milk, almond milk, or macadamia milk on hand
- Read labels carefully: Check plant-based milk ingredients for added gums or high FODMAP fibers
- Avoid instant blends: Skip coffee mixes containing chicory or added fibers
When selecting plant-based milk alternatives, look for products with minimal ingredients. Some brands add gums, emulsifiers, or fibers that might cause digestive issues in sensitive individuals, even if they're technically low FODMAP.
At Cafés and On the Go
Ordering coffee while following a low FODMAP diet requires some strategy, but it's entirely manageable with these approaches:
Café Ordering Strategy
- Request lactose-free or plant-based milk when available
- Ask for milk/creamer on the side to control quantity
- Avoid flavored lattes and specialty drinks
- Skip whipped cream and flavored syrups
- Choose simple preparations: americano, black coffee, or plain espresso
Many coffee shops now offer lactose-free milk, almond milk, or oat milk alternatives. However, be cautious with oat milk, as it can be high FODMAP in larger quantities. When in doubt, ask for the milk on the side so you can control the amount.
Hidden Ingredients Alert: Pre-mixed drinks, flavored lattes, and barista-added syrups often contain high FODMAP ingredients. Stick to simple preparations when you can't verify all ingredients.
Managing Quantity and Symptoms
Even with low FODMAP ingredients, individual tolerance varies significantly. Here's how to find your optimal coffee consumption:
Start Small and Build: Begin with a small espresso or half-cup of brewed coffee. Monitor your symptoms for 2-3 hours, then gradually increase serving sizes as tolerated.
Keep a Symptom Diary: Track coffee consumption alongside digestive symptoms. Note the type of coffee, amount consumed, timing, and any additives used. This data helps identify patterns and optimal consumption timing.
Consider Professional Guidance: Working with a FODMAP-trained dietitian provides personalized support for managing coffee within your overall dietary plan. They can help you systematically test tolerance while ensuring nutritional needs are met.
Remember that coffee tolerance can change based on stress levels, sleep quality, and overall gut health. What works during calm periods might not work during stressful times, so stay flexible with your approach.
Coffee Isn't the Only Non-FODMAP Trigger
Understanding that coffee can trigger IBS symptoms without being high FODMAP opens up a broader conversation about digestive health. Many foods and beverages can cause discomfort through mechanisms completely separate from FODMAP content.
The low FODMAP diet addresses one specific type of digestive trigger—fermentable carbohydrates. However, IBS symptoms can stem from multiple sources, including caffeine sensitivity, food intolerances, and individual gut responses.
Other Common Non-FODMAP IBS Triggers
Beyond coffee's stimulatory effects, several other foods and beverages can trigger IBS symptoms through non-FODMAP pathways:
- Alcohol
- Increases gut motility and can disrupt the gut microbiome, leading to digestive upset regardless of FODMAP content
- High-Fat Foods
- Trigger the gastrocolic reflex, causing rapid intestinal contractions that can lead to urgency and cramping
- Carbonated Beverages
- Introduce gas directly into the digestive system, potentially causing bloating and discomfort
- Spicy Foods
- Contain capsaicin and other compounds that can irritate the digestive tract and increase motility
- Artificial Sweeteners
- Some sugar alcohols like sorbitol are high FODMAP, but others may cause symptoms through different mechanisms
Research Insight: Studies show that up to 70% of people with IBS have food triggers beyond FODMAPs. This highlights why a comprehensive approach to dietary management often works better than focusing solely on FODMAP elimination.
Strategies for Managing Non-FODMAP Triggers
Successfully managing IBS often requires addressing multiple trigger types simultaneously. Here's how to approach non-FODMAP triggers systematically:
- Identify triggers through systematic testing: Work with a healthcare professional to test one variable at a time
- Monitor timing and context: Note when symptoms occur relative to meals, stress levels, and sleep quality
- Adjust portions before eliminating: Sometimes reducing quantity rather than complete avoidance is sufficient
- Address lifestyle factors: Stress, sleep, and physical activity all influence gut sensitivity
- Consider preparation methods: How food is cooked or processed can affect digestibility
"We've found that our customers often have the best success when they view their digestive health holistically. The low FODMAP diet is an excellent starting point, but paying attention to stress management, meal timing, and other food sensitivities creates a more complete picture."
Coffee's relationship with IBS symptoms perfectly illustrates this complexity. While the beverage itself is low FODMAP, its caffeine content, acidity, and individual tolerance factors all play roles in how it affects digestive comfort.
Professional Guidance: Working with a FODMAP-trained dietitian helps you navigate both FODMAP and non-FODMAP triggers systematically, ensuring you don't unnecessarily restrict your diet while still managing symptoms effectively.
Summary and Expert Recommendations
The relationship between coffee and digestive health illustrates perfectly why understanding FODMAPs requires nuance. Coffee itself is definitively low FODMAP, but it may still trigger IBS symptoms through entirely different mechanisms—primarily its stimulant properties and acidity.
For anyone asking "is coffee low FODMAP?"—yes, pure coffee contains no fermentable carbohydrates and is considered safe on the low FODMAP diet. However, individual tolerance varies significantly based on caffeine sensitivity and gut health.
The key insights for coffee lovers managing digestive sensitivity include:
- Pure coffee is your friend: Black coffee, espresso, and quality instant coffee are all low FODMAP choices
- Additives matter most: Problems typically arise from dairy milk, certain plant milks, and flavored syrups
- Portion control helps: Even low FODMAP foods can cause issues in large quantities
- Individual testing is crucial: Your tolerance may differ significantly from others
Coffee on Low FODMAP Diet: Quick Reference
- ✅ Black coffee, espresso, cold brew
- ✅ Lactose-free milk, almond milk, macadamia milk
- ✅ Regular sugar, maple syrup
- ✅ Decaf options for caffeine-sensitive individuals
- ❌ Regular dairy milk
- ❌ Whole soybean-based soy milk
- ❌ Honey, agave, artificial sweeteners with sugar alcohols
For those following a low FODMAP diet, coffee represents an excellent example of how to maintain enjoyment while supporting digestive health. The beverage's low FODMAP status means you don't need to eliminate it entirely—instead, focus on smart preparation choices and mindful consumption.
Remember that managing IBS and digestive sensitivity is highly individual. What works for one person may not work for another, and your tolerance can change based on stress, sleep, and overall gut health. Stay flexible and patient with your approach.
At Gourmend Foods, we understand that navigating dietary restrictions while maintaining flavor and enjoyment requires both knowledge and high-quality ingredients. Just as we've created low FODMAP broths and seasonings that don't sacrifice taste, you can continue enjoying coffee by making informed choices about preparation and additives.
Whether you're starting your low FODMAP journey or fine-tuning your existing approach, coffee can remain part of your daily routine. Focus on pure ingredients, listen to your body, and don't hesitate to seek professional guidance when needed. Your perfect cup of coffee—one that's both delicious and digestively comfortable—is absolutely achievable.
Check out our Low Fodmap Bundles
Frequently Asked Questions
Can I drink coffee on a low FODMAP diet?
Yes, you can enjoy coffee on a low FODMAP diet, but in moderation. Black coffee is generally low FODMAP in typical serving sizes because it doesn’t contain fermentable carbs. However, adding high FODMAP ingredients like milk or flavored syrups can trigger symptoms, so it’s best to stick with plain coffee or use low FODMAP milk alternatives like lactose-free or almond milk.
What kind of coffee is OK for IBS?
For IBS, plain black coffee or espresso is usually well tolerated in moderate amounts. Avoid coffee drinks with high FODMAP add-ins such as regular milk, whipped cream, or high-fructose syrups. Cold brew coffee can sometimes be easier on digestion due to lower acidity, and using low FODMAP milk alternatives helps keep it gut-friendly.
Is anything at Starbucks low FODMAP?
Yes, some Starbucks drinks can fit within a low FODMAP approach if you choose carefully. Opt for plain brewed coffee or espresso shots without dairy or flavored syrups. You can customize drinks with lactose-free or almond milk and skip the sweeteners. Avoid popular high FODMAP ingredients like regular milk, vanilla syrup, or caramel drizzle to keep symptoms at bay.
What drinks are FODMAP friendly?
FODMAP friendly drinks include water, plain black coffee, herbal teas without high FODMAP ingredients, lactose-free milk, almond milk, and certain fruit juices like cranberry or pineapple in small amounts. Sparkling water and green tea are also great options. Avoid drinks with high fructose corn syrup, honey, or dairy unless lactose-free.
Does IBS get worse with coffee?
Coffee can worsen IBS symptoms for some people because it stimulates the gut and can increase acid production. It may cause cramping, diarrhea, or discomfort, especially if consumed in large amounts. However, tolerance varies—many find that moderate amounts of plain coffee don’t trigger symptoms, especially when avoiding high FODMAP add-ins.
Is peanut butter low in FODMAP?
Yes, peanut butter is considered low FODMAP when consumed in moderate servings, typically about 2 tablespoons. It’s a good source of protein and healthy fats without fermentable carbs that trigger IBS symptoms. Just be sure to choose natural peanut butter without added high FODMAP ingredients like honey or high fructose corn syrup.